From the National Institute of Mental Health:
Bipolar disorder, also known as manic-depressive illness, is a brain disorder that causes unusual shifts in mood, energy, activity levels, and the ability to carry out day-to-day tasks. Symptoms are different from the normal ups and downs that everyone goes through from time to time. Bipolar disorder often develops in a person’s late teens or early adult years. At least half of all cases start before age 25.
Symptoms
People with bipolar disorder experience unusually intense emotional states that occur in distinct periods called mood episodes. An overly joyful or overexcited state is called a manic episode, and an extremely sad or hopeless state is called a depressive episode. Sometimes, a mood episode includes symptoms of both mania and depression. This is called a mixed state. People with bipolar disorder also may be explosive and irritable during a mood episode. Most people experience symptoms along a spectrum rather than only at the extremes.
Manic Episode Symptoms
Mood Changes
- A long period of feeling high, or an overly happy or outgoing mood
- Extremely irritable mood, agitation, feeling jumpy or wired.
Behavioral Changes
- Talking very fast, jumping from one idea to another, having racing thoughts
- Being easily distracted
- Increasing goal-directed activities, such as taking on new projects
- Being restless
- Sleeping little
- Having an unrealistic belief in one’s abilities
- Behaving impulsively and taking part in a lot of pleasurable,
high-risk behaviors, such as spending sprees, impulsive sex, and impulsive business investments.
Depressive Episode Symptoms
Mood Changes
- A long period of feeling worried or empty
- Loss of interest in activities once enjoyed, including sex.
Behavioral Changes
- Feeling tired or slowed down
- Having problems concentrating, remembering, and making decisions
- Being restless or irritable
- Changing eating, sleeping, or other habits
- Thinking of death or suicide, or attempting suicide.
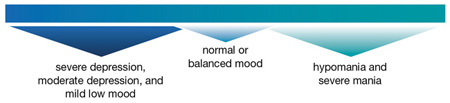
One side of the scale includes severe depression, moderate depression, and mild low mood. Moderate depression may cause less extreme symptoms, and mild low mood is called dysthymia when it is chronic or long-term. In the middle of the scale is normal or balanced mood.
At the other end of the scale are hypomania and severe mania. During hypomanic episodes, a person may have increased energy and activity levels that are not as severe as typical mania, or he or she may have episodes that last less than a week and do not require emergency care. A person having a hypomanic episode may feel very good, be highly productive, and function well. This person may not feel that anything is wrong even as family and friends recognize the mood swings as possible bipolar disorder.
During a mixed state, symptoms often include agitation, trouble sleeping, major changes in appetite, and suicidal thinking. People in a mixed state may feel very sad or hopeless while feeling extremely energized.
Doctors usually diagnose mental disorders using guidelines from the Diagnostic and Statistical Manual of Mental Disorders, or DSM. According to the DSM, there are four basic types of bipolar disorder:
- Bipolar I Disorder is mainly defined by manic or mixed episodes that last at least seven days, or by manic symptoms that are so severe that the person needs immediate hospital care. The symptoms of mania or depression must be a major change from the person’s normal behavior.
- Bipolar II Disorder is defined by a pattern of depressive episodes shifting back and forth with hypomanic episodes, but no full-blown manic or mixed episodes.
- Bipolar Disorder Not Otherwise Specified (BP-NOS) is diagnosed when a person has symptoms of the illness that do not meet diagnostic criteria for either bipolar I or II. However, the symptoms are clearly out of the person’s normal range of behavior.
- Cyclothymic Disorder, or Cyclothymia, is a mild form of bipolar disorder. People who have cyclothymia have episodes of hypomania that shift back and forth with mild depression for at least two years.
Some people may be diagnosed with rapid-cycling bipolar disorder. This is when a person has four or more episodes of major depression, mania, hypomania, or mixed symptoms within a year. Some people experience more than one episode in a week, or even within one day. Rapid cycling seems to be more common in people who have severe bipolar disorder and may be more common in people who have their first episode at a younger age. One study found that people with rapid cycling had their first episode about four years earlier, during mid to late teen years, than people without rapid cycling bipolar disorder. Rapid cycling affects more women than men.
Comorbidity (companion disorders)
Substance abuse is very common among people with bipolar disorder. However, substance abuse may trigger or prolong bipolar symptoms, and the behavioral control problems associated with mania can result in a person drinking too much.
Anxiety disorders, such as post-traumatic stress disorder (PTSD) and social phobia, also co-occur often among people with bipolar disorder. Bipolar disorder also co-occurs with attention deficit hyperactivity disorder (ADHD), which has some symptoms that overlap with bipolar disorder, such as restlessness and being easily distracted.
People with bipolar disorder are also at higher risk for thyroid disease, migraine headaches, heart disease, diabetes, obesity, and other physical illnesses. These illnesses may cause symptoms of mania or depression. They may also result from treatment for bipolar disorder.
Other illnesses can make it hard to diagnose and treat bipolar disorder. People with bipolar disorder should monitor their physical and mental health.
Diagnosis and Treatment
There is currently no test for bipolar disorder, despite genetic and brain structure factors, and no cure. Treatment involves reduction in severity of symptoms through psychotherapy and medication. Reactions to medications are unpredictable, and the best treatment is usually found through trial and error. Since mood stabilization is a primary focus, many people choose to pursue natural therapies, including light, exercise, diet, meditation, herbs, and affirmation. Others pursue more western forms of treatment, including anti-psychotics, anti-depressants, and psychotherapy.
Continue reading at the original source →